Surveillance: Notes on Genetic Sequencing and Cluster Detection Technologies: MPH Practicum Project Proposal Idea
I recently read through the CDC's DETECTING AND RESPONDING TO HIV TRANSMISSION CLUSTERS: A GUIDE FOR HEALTH DEPARTMENTS (2018), and have more questions than I began with, especially regarding the scope of technological functions and surveillance strategies, the ethical implications and social effects in prioritized populations, and the cultural toll it will have in the minoritized community with a history of mistrust for public health institutions.
Medical Monitoring Project( VDH Stakeholder Meeting: 2015)
-Ongoing supplemental surveillance system assessing behaviors and clinical characteristics of persons w/HIV who have received outpatient HIV medical care.
-To learn more about the experiences and needs of people receiving care
-Funded by CDC
HIV Incidence Surveillance
- Provides estimates of the number of new HIV infection over a certain period of time.
- Incidence refers to persons newly infected with HIV in a specified time period, whereas a person newly diagnosed with H IV may have been infected for years before diagnosed.
Molecular HIV Surveillance
-Collect all HIV nucleotide sequence data from laboratories that perform HIV genotypic drug resistance testing;
- What regulations need to be changed to facilitate full implementation of this project?
- Assess HIV drug resistance, evaluate HIV genetic diversity, and describe HIV transmission patterns.
Molecular HIV Surveillance
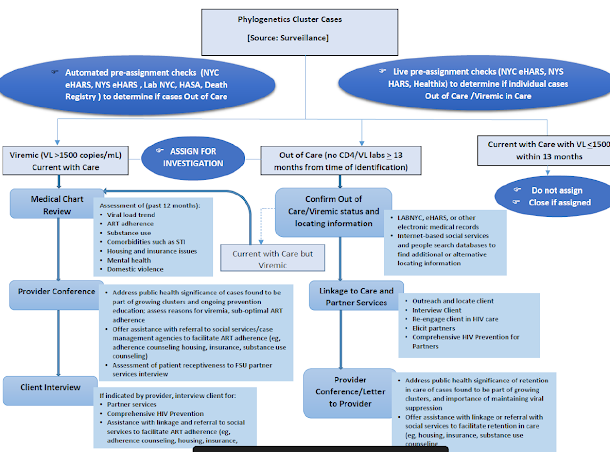
Surveillance staff examine how closely related different viruses are based on the similarities and differences between the DNA sequence patterns. When combined with information on a person’s demographics, geographic location, and risk characteristics, this analysis can help describe likely transmission patterns between persons. There is much debate about whether clear directionality can be determined. Analysis of these transmission patterns or networks can help guide HIV prevention efforts and optimize the allocation of resources by identifying persons at highest risk of being infected with HIV. Identifying active HIV transmission is key in HIV prevention and care efforts. It is important to identify growing clusters in order interrupt transmission.
Comments
Post a Comment